एपेन्डिसाइटिस
| ICD-10 | K35. - K37. | |
|---|---|---|
| ICD-9 | 540-543 | |
| DiseasesDB | 885 | |
| मेडलाइन प्लस | 000256 | |
| ईमेडिसिन | med/3430 emerg/41 ped/127 ped/2925 | |
| MeSH | C06.405.205.099 | |
एपेन्डिसाइटिस भर्मिफर्म एपेन्डिक्स इन्फ्लामेसन जुइगु छगु अवस्था खः[१]। थ्व अवस्थायु माइल्ड केसतेत छुं हे मयासें नं लनेफु धासा सिक्क हे तच्वगु अवस्थाय् इन्फ्लेम्ड एपेन्डिक्सयात ल्यापारोटोमी वा ल्यापारोस्कोपी याना लिकाय् माली। थ्व अवस्था मलंकुसा मनु पेरिटोनाइटिस व शकय् वना सी तक्क नं फु।[२]
ल्वेजुइगु कारण
[सम्पादन]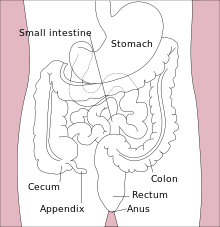
The appendix loses the ability to fight infection and fecal bacteria begin to grow out of control. Although spontaneous recovery can rarely occur, with time and lack of treatment the walls of the appendix eventually become gangrenous from the infection and lack of blood flow. As bacteria begin to leak out through the dying walls, pus forms within and around the appendix (suppuration). The end result of this cascade is appendiceal rupture causing peritonitis, which may lead to septicemia and eventually death.
Although the model described above is traditionally taught in medical schools, histories of patients operated for appendicitis do not often correlate well with such a single disease progression. Specifically, those with atypical histories have findings at surgery that are consistent with a suppurative process that starts at the onset of symptoms and then smolders. Patients with typical histories may have findings suggesting resolution. Histories to suggest rupture of the appendix while patients are being diagnostically observed are exceedingly rare.
Thus appendicitis is now considered by some to behave as two distinct disease processes, typical and atypical (or suppurative). Approximately two-thirds of patients with appendicitis have typical histories, and findings suggest a virus or mild obstruction as a cause. In the third with atypical histories, an early suppurative process begins at the clinical onset, and severe unremitting obstruction is the likely cause. In any case, early surgical removal is the best treatment for either type of appendicitis. (Hobler,K., 1998)
Appendicitis’ apparently idiopathic nature has led to many different theories explaining its occurrence. One theory regarding the cause of appendicitis, sometimes facetiously referred to as "the porcelain throne theory”, was proposed by Dr. Denis Burkitt, who developed the theory after observing low rates of appendicitis in Uganda. He proposed two causes for this: one, the Africans ate a diet high in fiber, and two, they used squat toilets rather than seat toilets. Most health practitioners accept Dr. Burkitt's first cause as a contributing factor, but are unfamiliar with the second one, which has never been tested.
A third hypothesis, which has gained less attention, proposes that a lack of adequate sanitary facilities in the developing world may actually have a protective effect against later appendicitis. This theory, proposed by Baker in 1985, hypothesized that infants in the developed world are exposed to fewer enteric organisms, which modifies their immune response to virus infections, which might then cause appendicitis. This is also unverified. [१]
साइन, सिम्प्टम व फाइन्डिंग
[सम्पादन]Appendicitis can be classified into two types, typical and atypical. The pain of typical acute appendicitis usually starts centrally (periumbilical) before localising to the right iliac fossa (the lower right side of the abdomen). There is usually associated loss of appetite (anorexia) and fever. Nausea, or vomiting may or may not occur. These classic signs and symptoms are more likely in younger patients. Older patients (beyond their teenage years) may present with only one or two. Diagnosis is easier in typical acute appendicitis and surgery removes a swollen appendix with little or no suppuration (pus) if operated early (within 24 hours of onset).
Atypical histories are not unusual and are more often associated with suppurative appendicitis. This condition often starts with right lower quadrant pain and may smolder with non-specific symptoms (e.g.,malaise,lethargy and/or fever) for several days before a diagnosis of appendicitis can be made. Diarrhea, a symptom of gastroenteritis, may occur if the appendiceal inflammation irritates adjacent intestine. Diagnosis is more difficult and surgery removes an appendix that is suppurative, gangrenous or ruptured.
There is typically pain and tenderness in the right iliac fossa in both typical and atypical (suppurative) appendicitis. Rebound tenderness may be present suggesting that there is some element of peritoneal irritation. Asking the patient to cough gently and point to the tender spot is the least painful way to localize the area of peritonitis. If the abdomen is involuntarily guarded (rigid), there should be a strong suspicion of peritonitis requiring urgent surgical intervention.
डायग्नोसिस
[सम्पादन]Diagnosis is based on history and physical examination backed by an elevation of neutrophilic white cells, and other infection markers on blood testing and imaging.
The classical history in appendicitis is diffuse pain in the periumbilical region which then localizes as pain and tenderness at McBurney's point (associated with an inflamed appendix coming in contact with the surrounding parietal peritoneum). This point is located on the right-hand side of the abdomen one-third of the distance between the anterior superior iliac spine and the navel. Here, on gentle palpation, the abdominal muscles often feel firm to rigid because of involuntary spasm, and a cough also produces a localized soreness.
Other physical findings include right-side tenderness on a digital rectal exam. Since the appendix normally lies on the right, if a finger is inserted into the rectum and there is tenderness when pressure is applied toward the right, this indicates an increased likelihood that the patient has appendicitis.
Other signs used in the diagnosis of appendicitis are the psoas sign (useful in retrocecal appendicitis), the obturator sign (specifically the obturator internus muscle), Blumberg's sign, and Rovsing's sign.
Ultrasonography and Doppler sonography also provide useful means to detect appendicitis, especially in children. In some cases (15% approximately), however, ultrasonography of the iliac fossa does not reveal any abnormalities despite the presence of appendicitis. This is especially true of early appendicitis before the appendix has become significantly distended and in adults where larger amounts of fat and bowel gas make actually seeing the appendix technically difficult. Despite these limitations, in experienced hands sonographic imaging can often distinguish between appendicitis and other diseases with very similar symptoms such as inflammation of lymph nodes near the appendix or pain originating from other pelvic organs such as the ovaries or fallopian tubes.
In places where it is readily available, CT scan has become the diagnostic test of choice, especially in adults. A properly performed CT scan with modern equipment has a detection rate (sensitivity) of over 95% and a similar specificity. Signs of appendicitis on CT scan include lack of contrast (oral dye) in the appendix and direct visualization of appendiceal enlargement (greater than 6 mm in diameter on cross section). The inflammation caused by appendicitis in the surrounding peritoneal fat (so called "fat stranding") can also be observed on CT, providing a mechanism to detect early appendicitis and a clue that appendicitis may be present even when the appendix is not well seen. Thus, diagnosis of appendicitis by CT is made more difficult in very thin patients and in children, both of whom tend to lack significant fat within the abdomen. In most cases, however, appendicitis is a clinical diagnosis and, due to the high radiation dose involved, CT scans are only used when the diagnosis is in doubt (e.g. atypical history) or if there are other considerations involved.
चिकित्सा
[सम्पादन]चिकित्सा अप्व याना शल्यचिकित्सा यागु माध्यमं जुइ। Appendicitis can be treated by removal of the appendix through a surgical procedure called an appendicectomy (also known as an appendectomy). The incision of appendectomy can be a Gridiron incision, a Lanz incision, or the midline incision.
Often now the operation can be performed via a laparoscopic approach, or via small incisions with a camera to visualize the area of interest in the abdomen. If the findings reveal suppurative appendicitis with complications such as rupture, abscess, adhesions, etc., conversion to open laparotomy may be necessary.
Antibiotics are often given intravenously to help kill remaining bacteria and thus reduce the incidence of infectious complication in the abdomen or wound.
प्रोग्नोसिस
[सम्पादन]Most appendicitis patients recover easily with treatment, but complications can occur if treatment is delayed or if peritonitis occurs.
Recovery time depends on age, condition, complications, and other circumstances but usually is between 10 and 28 days.
The real possibility of life-threatening peritonitis is the reason why acute appendicitis warrants speedy evaluation and treatment. The patient may have to undergo a medical evacuation. Appendectomies have occasionally been performed in emergency conditions (i.e. outside of a proper hospital), when a timely medical evacuation was impossible.
Typical acute appendicitis responds quickly to appendectomy and occasionally will resolve spontaneously. If appendicitis resolves spontaneously, it remains controversial whether an elective interval appendectomy should be performed to prevent a recurrent episode of appendicitis. Atypical appendicitis (associated with suppurative appendicitis) is more difficult to diagnose and is more apt to be complicated even when operated early. In either condition prompt diagnosis and appendectomy yield the best results with full recovery in two to four weeks usually. Mortality and severe complications are unusual but do occur, especially if peritonitis persists untreated.
श्रोतs
[सम्पादन]- ↑ The American Heritage Stedman's Medical Dictionary. KMLE Medical Dictionary Definition of appendicitis.
- ↑ Hobler, K., Acute and Suppurative Appendicitis: Disease Duration and its Implications for Quality Improvement, Permanente Medical Journel, volume 2, #2, Spring 1998.
पिनेयागु स्वापूतः
[सम्पादन]- Appendicitis - MayoClinic.com, from the Web site of the Mayo Clinic
- The Merck Manual of Diagnosis and Therapy: Appendicitis
- Appendicitis Research Latest research from the literature on appendicitis
- Acute and Suppurative Appendicitis
| विकिमिडिया मंका य् थ्व विषय नाप स्वापु दुगु मिडिया दु: Appendicitis |
